Abstract
Purpose
Our aim is to establish an AI model for distinguishing color fundus photographs (CFP) of RVO patients from normal individuals.
Methods
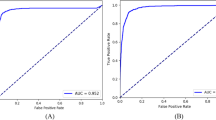
The training dataset included 2013 CFP from fellow eyes of RVO patients and 8536 age- and gender-matched normal CFP. Model performance was assessed in two independent testing datasets. We evaluated the performance of the AI model using the area under the receiver operating characteristic curve (AUC), accuracy, precision, specificity, sensitivity, and confusion matrices. We further explained the probable clinical relevance of the AI by extracting and comparing features of the retinal images.
Results
Our model achieved an average AUC was 0.9866 (95% CI: 0.9805–0.9918), accuracy was 0.9534 (95% CI: 0.9421–0.9639), precision was 0.9123 (95% CI: 0.8784–9453), specificity was 0.9810 (95% CI: 0.9729–0.9884), and sensitivity was 0.8367 (95% CI: 0.7953–0.8756) for identifying fundus images of RVO patients in training dataset. In independent external datasets 1, the AUC of the RVO group was 0.8102 (95% CI: 0.7979–0.8226), the accuracy of 0.7752 (95% CI: 0.7633–0.7875), the precision of 0.7041 (95% CI: 0.6873–0.7211), specificity of 0.6499 (95% CI: 0.6305–0.6679) and sensitivity of 0.9124 (95% CI: 0.9004–0.9241) for RVO group. There were significant differences in retinal arteriovenous ratio, optic cup to optic disc ratio, and optic disc tilt angle (p = 0.001, p = 0.0001, and p = 0.0001, respectively) between the two groups in training dataset.
Conclusion
We trained an AI model to classify color fundus photographs of RVO patients with stable performance both in internal and external datasets. This may be of great importance for risk prediction in patients with retinal venous occlusion.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
References
Ip M, Hendrick A. Retinal vein occlusion review. Asia Pac J Ophthalmol (Philos). 2018;7:40–5.
Rogers S, McIntosh R, Cheung N, Lim L, Wang J, Mitchell P, et al. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology. 2010;117:313–9.e1.
Di Capua M, Coppola A, Albisinni R, Tufano A, Guida A, Di Minno MN, et al. Cardiovascular risk factors and outcome in patients with retinal vein occlusion. J Thromb Thrombolysis. 2010;30:16–22.
Hayreh SS, Zimmerman B, McCarthy MJ, Podhajsky P. Systemic diseases associated with various types of retinal vein occlusion. Am J Ophthalmol. 2001;131:61–77.
Hirano Y, Suzuki N, Tomiyasu T, Kurobe R, Yasuda Y, Esaki Y, et al. Multimodal imaging of microvascular abnormalities in retinal vein occlusion. J. Clin. Med. 2021;10:405.
Kim MJ, Woo SJ, Park KH, Kim TW. Retinal nerve fiber layer thickness is decreased in the fellow eyes of patients with unilateral retinal vein occlusion. Ophthalmology. 2011;118:706–10.
Maltsev DS, Kulikov AN, Burnasheva MA, Chhablani J. Prevalence of resolved paracentral acute middle maculopathy lesions in fellow eyes of patients with unilateral retinal vein occlusion. Acta Ophthalmol. 2020;98:e22–e28.
Arslan GD, Guven D, Demir M, Alkan AA, Ozcan D. Microvascular and functional changes according to the fundus location of the affected arteriovenous crossing in patients with branch retinal vein occlusion. Indian J Ophthalmol. 2021;69:1189–96.
Pinhas A, Dubow M, Shah N, Cheang E, Liu CL, Razeen M, et al. FELLOW EYE CHANGES IN PATIENTS WITH NONISCHEMIC CENTRAL RETINAL VEIN OCCLUSION: Assessment of Perfused Foveal Microvascular Density and Identification of Nonperfused Capillaries. Retina. 2015;35:2028–36.
Shin YI, Nam KY, Lee SE, Lim HB, Lee MW, Jo YJ, et al. Changes in peripapillary microvasculature and retinal thickness in the fellow eyes of patients with unilateral retinal vein occlusion: An OCTA study. Invest Ophthalmol Vis Sci. 2019;60:823–9.
Lim SH, Kim M, Chang W, Sagong M. Comparison of the lamina cribrosa thickness of patients with unilateral branch retinal vein occlusion and healthy subjects. Retina. 2017;37:515–21.
Chan MMH, Thomas AS, Yoon SP, Leitner D, Fekrat S. Clinical characteristics of patients with CRVO in one eye with subsequent RVO in the fellow eye: a retrospective observational study. Ophthalmic Surg, lasers Imaging Retin. 2019;50:444–9.
McIntosh RL, Rogers SL, Lim L, Cheung N, Wang JJ, Mitchell P, et al. Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010;117:1113–1123 e15.
Sakaue H, Katsumi O, Hirose T. Electroretinographic findings in fellow eyes of patients with central retinal vein occlusion. Arch Ophthalmol. 1989;107:1459–62.
Ferraz DA, Tovar-Moll F, Belfort R Jr. Artificial intelligence: from the retina to the brain. Arq Bras Oftalmol. 2021;84:197–198.
Date RC, Jesudasen SJ, Weng CY. Applications of deep learning and artificial intelligence in retina. Int Ophthalmol Clin. 2019;59:39–57.
Schmidt-Erfurth U, Sadeghipour A, Gerendas BS, Waldstein SM, Bogunovic H. Artificial intelligence in retina. Prog Retin Eye Res. 2018;67:1–29.
Zhang Y, Shi J, Peng Y, Zhao Z, Zheng Q, Wang Z, et al. Artificial intelligenceenabled screening for diabetic retinopathy: a real-world, multicenter and prospective study. BMJ Open Diab Res Care 2020;8:e001596.
Yim J, Chopra R, Spitz T, Winkens J, Obika A, Kelly C, et al. Predicting conversion to wet age-related macular degeneration using deep learning. Nat Med. 2020;26:892–9.
Prabhakar B, Singh RK, Yadav KS. Artificial intelligence (AI) impacting diagnosis of glaucoma and understanding the regulatory aspects of AI-based software as medical device. Comput Med Imaging Graph. 2020;87:101818.
Li JO, Liu H, Ting DSJ, Jeon S, Chan RVP, Kim JE, et al. Digital technology, tele-medicine and artificial intelligence in ophthalmology: A global perspective. Prog Retin Eye Res. 2021;82:100900.
Goldhagen BE, Al-Khersan H. Diving deep into deep learning: an update on artificial intelligence in retina. Curr Ophthalmol Rep. 2020;8:121–8.
Adhi M, Filho MA, Louzada RN, Kuehlewein L, de Carlo TE, Baumal CR, et al. Retinal capillary network and foveal avascular zone in eyes with vein occlusion and fellow eyes analyzed with optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2016;57:OCT486–94.
Costanzo E, Parravano M, Gilardi M, Cavalleri M, Sacconi R, Aragona E, et al. Microvascular retinal and choroidal changes in retinal vein occlusion analyzed by two different optical coherence tomography angiography devices, ophthalmologica. J Int d’ophtalmologie Int J Ophthalmol Z fur Augenheilkd. 2019;242:8–15.
Chen L, Yuan M, Sun L, Wang Y, Chen Y. Evaluation of microvascular network with optical coherence tomography angiography (OCTA) in branch retinal vein occlusion (BRVO). BMC Ophthalmol. 2020;20:154.
Vieira MJ, Campos A, do Carmo A, Arruda H, Martins J, Sousa JP. Thrombophilic risk factors for retinal vein occlusion. Sci Rep. 2019;9:18972.
Stojakovic T, Scharnagl H, Marz W, Winkelmann BR, Boehm BO, Schmut O. Low density lipoprotein triglycerides and lipoprotein(a) are risk factors for retinal vascular occlusion. Clin Chim Acta. 2007;382:77–81.
Nagasato D, Tabuchi H, Ohsugi H, Masumoto H, Enno H, Ishitobi N, et al. Deep-learning classifier with ultrawide-field fundus ophthalmoscopy for detecting branch retinal vein occlusion. Int J Ophthalmol. 2019;12:94–99.
Nagasato D, Tabuchi H, Ohsugi H, Masumoto H, Enno H, Ishitobi N, et al. Deep neural network-based method for detecting central retinal vein occlusion using ultrawide-field fundus ophthalmoscopy. J Ophthalmol. 2018;2018:1875431.
Nagasato D, Tabuchi H, Masumoto H, Enno H, Ishitobi N, Kameoka M, et al. Automated detection of a nonperfusion area caused by retinal vein occlusion in optical coherence tomography angiography images using deep learning. PLoS One. 2019;14:e0223965.
Hayreh SS. Photocoagulation for retinal vein occlusion. Prog Retin Eye Res. 2021;85:100964.
Karska-Basta I, Kubicka-Trzaska A, Romanowska-Dixon B, Undas A. Thrombophilia—a risk factor of retinal vein occlusion?. Klin Ocz. 2013;115:29–33.
Yildirim C, Yaylali V, Tatlipinar S, Kaptanoglu B, Akpinar S. Hyperhomocysteinemia: a risk factor for retinal vein occlusion. Ophthalmologica. 2004;218:102–6.
Undas A, Kubicka-Trzaska A. Thrombophilia as a risk factor for central retinal vein occlusion. Klin Ocz. 2003;105:221–4.
Chan EW, Wong TY, Liao J, Cheung CY, Zheng YF, Wang JJ, et al. Branch retinal vein occlusion and optic nerve head topographic parameters: the Singapore Indian eye study. Br J Ophthalmol. 2013;97:611–6.
Szigeti A, Schneider M, Ecsedy M, Nagy ZZ, Recsan Z. Optic disc morphology in unilateral branch retinal vein occlusion using spectral domain optical coherence tomography. BMC Ophthalmol. 2015;15:178.
Acknowledgements
We thank the Chengdu Ikangguobin Health Examination Center for provide the color fundus photographs.
Funding
This work was supported by The Project of National Key Research and Development (No. 2018YFC1106103) to MZ and Post-Doctor Research Project, West China Hospital, Sichuan University (2021HXBH030) to XR. And Natural Science Foundation of Sichuan Province (No. 2022NSFSC1285) to XR.
Author information
Authors and Affiliations
Contributions
XR, BW, and MZ designed the study, directed the project, and interpreted the data. XR, YG, RR, YT, WF, LJ, LH, WX, XL, TW, and YC performed the experiments. GZ provided guidance for this project. XR wrote the paper, and YL, XF, GZ, and MZ contributed to editing. All authors contributed to the paper and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ren, X., Feng, W., Ran, R. et al. Artificial intelligence to distinguish retinal vein occlusion patients using color fundus photographs. Eye 37, 2026–2032 (2023). https://doi.org/10.1038/s41433-022-02239-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02239-4